The oldest hospital in California — the only one serving the diverse population of Chinatown — now gone.
The local hospital that the community counted on just … closed. In as effort to make up for the loss, the building will be repurposed as a recreation center.
A two-year-old hospital with state of the art equipment went from chef-inspired meals to closure in the blink of an eye.
JOANNE FROGGE, BidMed President | I have liquidated more hospitals than one could imagine. I have walked the eerily quiet halls, the silence punctuated only by obstinately beeping equipment. It’s a rare opportunity to see a hospital completely devoid of patients and staff, yet looking like everyone just stepped away from their station.
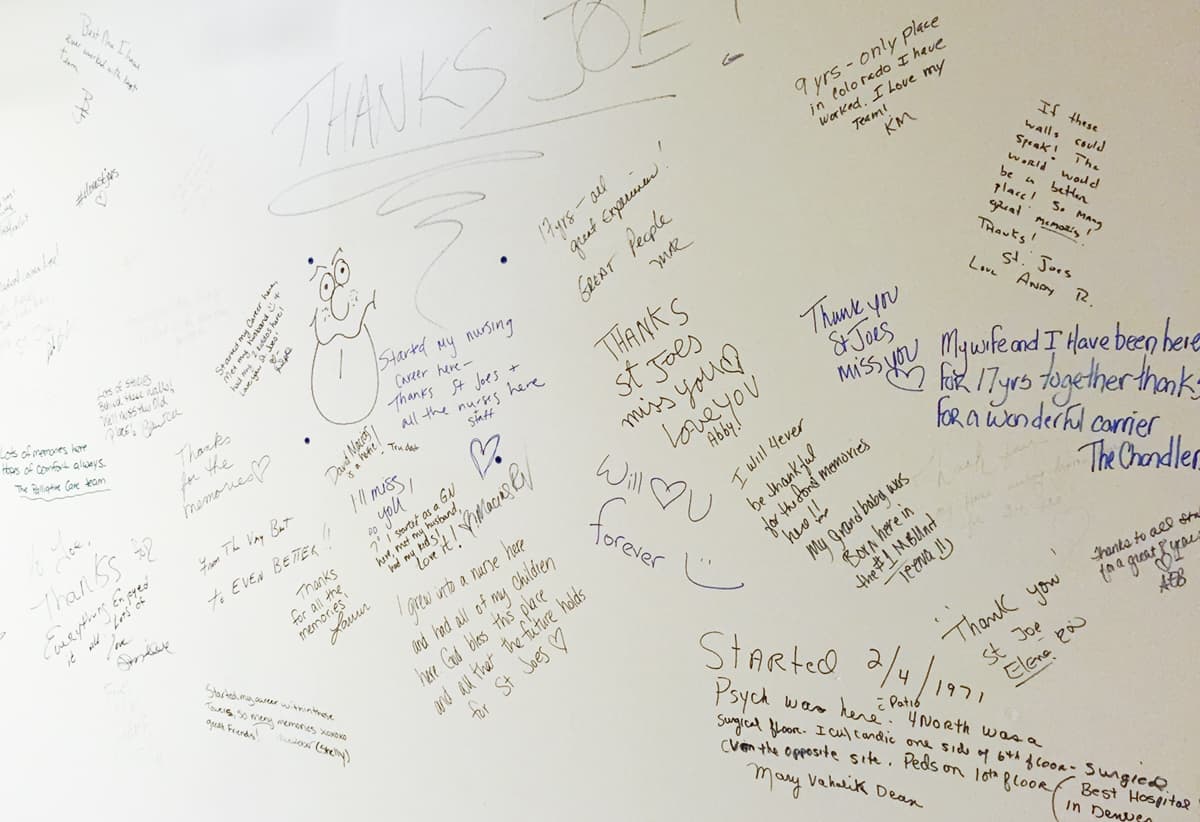
Messages are written on walls — reminders of a lifetime of memories experienced at that hospital. Patient white boards still display instructions, physician names, and goals for mom, like recognizing feeding cues with her baby. A beautiful white marble chapel serves as a consolidation area for equipment. For most seasoned hospital executives, this is a first-time experience in their career; but for me, it’s a typical project. The greatest assistance I can provide at this point is to guide them every step of the way, help maximize and recover the value that’s left, and empty their hospital. Even though I am in the business of closing down hospitals, it never feels right. The mission and vision statements are clearly emblazoned on the walls: to deliver the best care, relentlessly pursue excellent performance, and strive for continuous improvement and quality service. Where did these facilities go wrong?Cost Savings
 Strategic Sourcing Costs
Strategic Sourcing Costs
- New and Refurbished Capital
- Purchased Services
- Medical and Surgical Consumables and Supplies
- Capital Equipment Service Contracts
 Eliminate decision making inefficiencies using streamlined workflows
Eliminate decision making inefficiencies using streamlined workflows
 Volume pricing discounts from vendor contract consolidation
Volume pricing discounts from vendor contract consolidation
Cost Avoidance
 Additional costs that exceed evidence-based value
Additional costs that exceed evidence-based value
 Denied reimbursements due to insurance credentialing errors
Denied reimbursements due to insurance credentialing errors
 Fines resulting from compliance issues
Fines resulting from compliance issues
 Unintended renewals and fees due to poor contract lifecycle management
Unintended renewals and fees due to poor contract lifecycle management
 Unforeseen costs due to inadequate capital replacement planning
Unforeseen costs due to inadequate capital replacement planning
Revenue Opportunities
 Maximize reimbursement rates using the same clinical evidence as Payers
Maximize reimbursement rates using the same clinical evidence as Payers
 Expedite billing for new providers by shortening the enrollment and credentialing process
Expedite billing for new providers by shortening the enrollment and credentialing process
 Fines resulting from compliance issues
Fines resulting from compliance issues
 Increase returns from trade-ins and retired medical equipment
Increase returns from trade-ins and retired medical equipment